The plan focuses on educating staff about infectious diseases, emphasizing both theoretical understanding and practical compliance. The metrics serve as vital indicators of program success, such as the Training Completion Rate. Achieving a 90% completion rate ensures a baseline competence in handling infectious materials, crucial for healthcare settings.
Post-Training Assessment Scores provide insight into knowledge retention. With a benchmark of 75%, these scores help tailor future curriculum to address learning gaps, promoting a solid foundation of understanding.
PPE Usage Compliance is critical, aiming for 95% adherence, which minimizes the risk of disease transmission and ensures safety. Feedback from Participants gauges satisfaction and identifies areas for program enhancement, maintaining an average rating of 4 out of 5.
Lastly, the Incident Reporting Rate reflects the real-world application of training, with a goal to decrease incidents by 30%, thus indicating improved safety practices.
Top 5 metrics for Education on Infectious Diseases
1. Training Completion Rate
The percentage of staff who have completed the training program on infectious diseases and PPE preparations.
What good looks like for this metric: 90% completion rate
How to improve this metric:- Create a mandatory training schedule
- Send regular reminders to complete training
- Offer incentives for early completion
- Provide flexible training times
- Ensure easy access to training materials
2. Post-Training Assessment Scores
The average score of staff on assessments conducted after training to evaluate understanding and retention of information.
What good looks like for this metric: 75% average score
How to improve this metric:- Enhance the clarity of training materials
- Incorporate interactive learning methods
- Provide additional resources for self-study
- Offer review sessions or refresher courses
- Implement individualized feedback on assessments
3. PPE Usage Compliance
The percentage of staff correctly using PPE as per guidelines during drills or assessments.
What good looks like for this metric: 95% compliance
How to improve this metric:- Conduct regular PPE drills
- Provide clear PPE usage guidelines
- Supervise and guide during PPE drills
- Offer corrective training for non-compliance
- Use checklists for PPE usage
4. Feedback from Participants
The qualitative and quantitative feedback collected from staff about the effectiveness of the training program.
What good looks like for this metric: 4 out of 5 average rating
How to improve this metric:- Conduct anonymous surveys post-training
- Hold feedback sessions with experienced trainers
- Implement a feedback loop to improve training
- Encourage open communication for suggestions
- Act on feedback promptly to show responsiveness
5. Incident Reporting Rate
The number of infectious disease incidents reported and managed correctly post-training compared to pre-training.
What good looks like for this metric: Decrease by 30% post-training
How to improve this metric:- Improve ease of incident reporting procedures
- Encourage a culture of transparency and safety
- Highlight the importance of prompt reporting
- Facilitate regular training refresher sessions
- Analyse incident data to prevent future occurrences
How to track Education on Infectious Diseases metrics
It's one thing to have a plan, it's another to stick to it. We hope that the examples above will help you get started with your own strategy, but we also know that it's easy to get lost in the day-to-day effort.
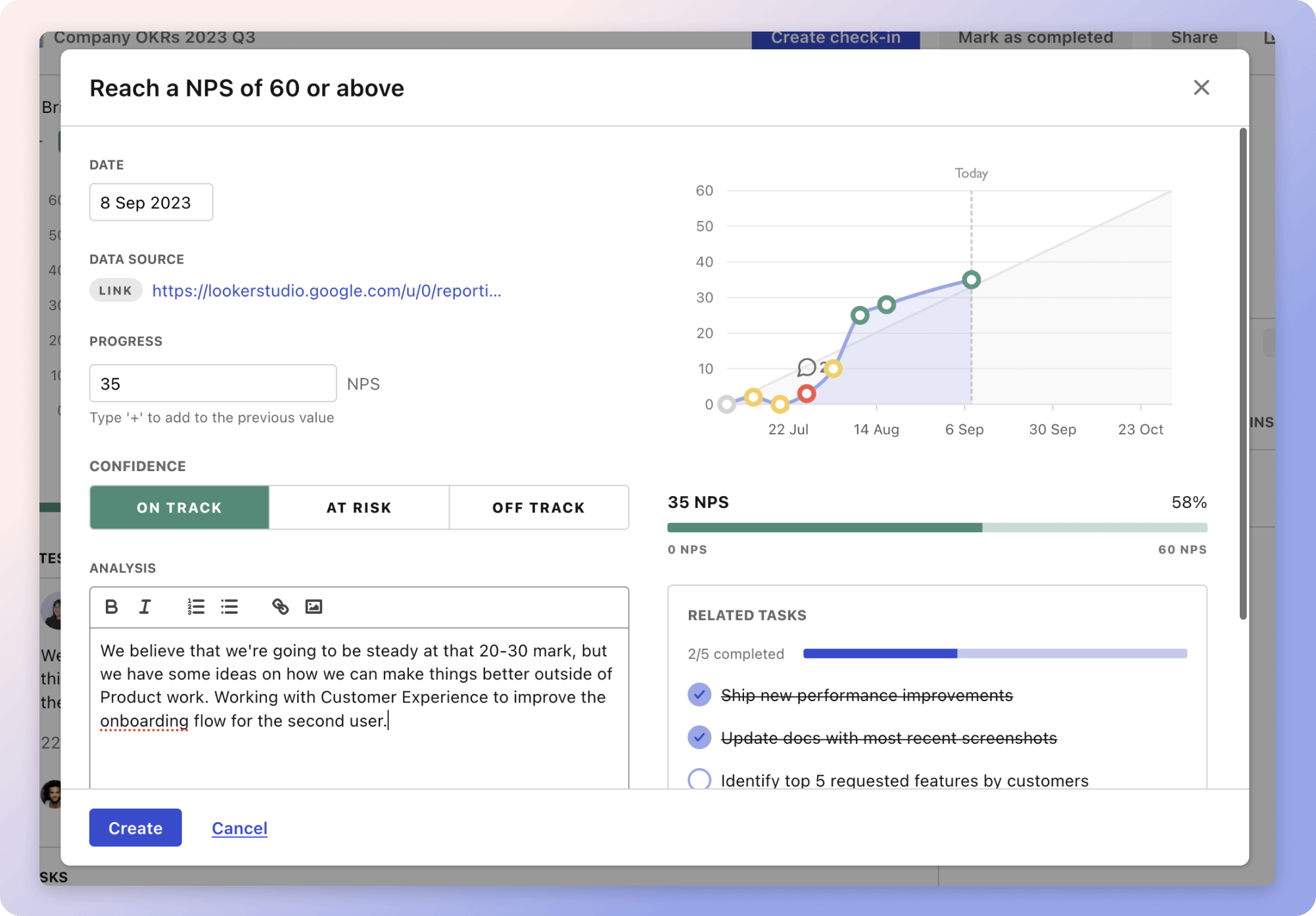
That's why we built Tability: to help you track your progress, keep your team aligned, and make sure you're always moving in the right direction.
Give it a try and see how it can help you bring accountability to your metrics.