What are Healthcare Staff metrics? Finding the right Healthcare Staff metrics can be daunting, especially when you're busy working on your day-to-day tasks. This is why we've curated a list of examples for your inspiration.
Copy these examples into your preferred tool, or adopt Tability to ensure you remain accountable.
Find Healthcare Staff metrics with AI While we have some examples available, it's likely that you'll have specific scenarios that aren't covered here. You can use our free AI metrics generator below to generate your own strategies.
Examples of Healthcare Staff metrics and KPIs 1. Hand Hygiene Compliance Rate The percentage of times clinical staff wash their hands following recommended guidelines
What good looks like for this metric: 80% compliance rate in healthcare settings
Ideas to improve this metric Implement regular staff training on hand hygiene Install more hand sanitiser dispensers Conduct random audits and provide immediate feedback Use visual cues or posters to remind staff Introduce a reward system for compliance 2. Contamination Incidence Rate The number of contamination events reported per 1,000 patient days
What good looks like for this metric: Less than 2 events per 1,000 patient days
Ideas to improve this metric Conduct thorough root cause analysis for each event Increase frequency of sanitation checks Enhance the usage of personal protective equipment Involve staff in contamination prevention strategies Regularly review and update infection control policies 3. Waste Segregation Accuracy Percentage of waste correctly segregated into appropriate categories
What good looks like for this metric: 95% correct segregation
Ideas to improve this metric Provide clear, colour-coded bins and labelling Train staff on waste segregation procedures Conduct waste audits to assess segregation accuracy Incorporate waste management into annual assessments Implement accountability measures for non-compliance 4. Staff Training Completion Rate Percentage of clinical staff who have completed required hygiene and waste management training
What good looks like for this metric: 100% completion annually
Ideas to improve this metric Schedule mandatory training sessions at convenient times Use online platforms for training flexibility Track and remind staff of training deadlines Encourage peer-to-peer knowledge sharing Provide certificates upon completion to acknowledge achievement 5. Patient Satisfaction Scores Related to Cleanliness Patient feedback scores on cleanliness and hygiene aspects of care
What good looks like for this metric: 4.5 out of 5 in patient satisfaction surveys
Ideas to improve this metric Solicit regular patient feedback and act on suggestions Improve visibility of cleaning efforts Ensure high-touch surfaces are sanitised frequently Engage patients in dialogue about hand hygiene Reward staff for high cleanliness scores
← →
1. Training Completion Rate The percentage of staff who have completed the training program on infectious diseases and PPE preparations.
What good looks like for this metric: 90% completion rate
Ideas to improve this metric Create a mandatory training schedule Send regular reminders to complete training Offer incentives for early completion Provide flexible training times Ensure easy access to training materials 2. Post-Training Assessment Scores The average score of staff on assessments conducted after training to evaluate understanding and retention of information.
What good looks like for this metric: 75% average score
Ideas to improve this metric Enhance the clarity of training materials Incorporate interactive learning methods Provide additional resources for self-study Offer review sessions or refresher courses Implement individualized feedback on assessments 3. PPE Usage Compliance The percentage of staff correctly using PPE as per guidelines during drills or assessments.
What good looks like for this metric: 95% compliance
Ideas to improve this metric Conduct regular PPE drills Provide clear PPE usage guidelines Supervise and guide during PPE drills Offer corrective training for non-compliance Use checklists for PPE usage 4. Feedback from Participants The qualitative and quantitative feedback collected from staff about the effectiveness of the training program.
What good looks like for this metric: 4 out of 5 average rating
Ideas to improve this metric Conduct anonymous surveys post-training Hold feedback sessions with experienced trainers Implement a feedback loop to improve training Encourage open communication for suggestions Act on feedback promptly to show responsiveness 5. Incident Reporting Rate The number of infectious disease incidents reported and managed correctly post-training compared to pre-training.
What good looks like for this metric: Decrease by 30% post-training
Ideas to improve this metric Improve ease of incident reporting procedures Encourage a culture of transparency and safety Highlight the importance of prompt reporting Facilitate regular training refresher sessions Analyse incident data to prevent future occurrences
← →
1. Completion Rate The percentage of history and physical exams completed within 24 hours of patient admission
What good looks like for this metric: 90-95%
Ideas to improve this metric Implement a reminder system for staff Introduce electronic health record alerts Provide training for efficient documentation Increase staffing during peak admission times Encourage early initiation of assessments 2. Average Completion Time The average time taken to complete history and physical exams after patient admission
What good looks like for this metric: Under 24 hours
Ideas to improve this metric Streamline documentation processes Utilise checklists for thoroughness and speed Cross-train staff for flexibility Optimise patient flow and prioritisation Regularly review and address bottlenecks 3. Staff Compliance Rate The percentage of staff adhering to the completion protocol for history and physical exams
What good looks like for this metric: Above 90%
Ideas to improve this metric Conduct routine compliance audits Offer incentives for high compliance Provide feedback on performance Strengthen compliance policies Ensure clarity in protocols and guidelines 4. Patient Outcome Correlation The link between timely completion of history and physical exams and patient outcomes
What good looks like for this metric: Positive correlation
Ideas to improve this metric Analyse correlations with patient recovery times Adjust practices based on outcome data Focus on accuracy and completeness in assessments Regularly reassess assessment procedures Align protocols with best practices 5. Error Rate in Documentation The frequency of errors found in the completed history and physical exams
What good looks like for this metric: Below 5%
Ideas to improve this metric Enhance staff training on documentation Introduce a peer review process Use electronic templates to minimise errors Implement regular quality checks Increase awareness of common documentation errors
← →
Tracking your Healthcare Staff metrics Having a plan is one thing, sticking to it is another.
Setting good strategies is only the first challenge. The hard part is to avoid distractions and make sure that you commit to the plan. A simple weekly ritual will greatly increase the chances of success.
A tool like Tability can also help you by combining AI and goal-setting to keep you on track.
More metrics recently published We have more examples to help you below.
Planning resources OKRs are a great way to translate strategies into measurable goals. Here are a list of resources to help you adopt the OKR framework:
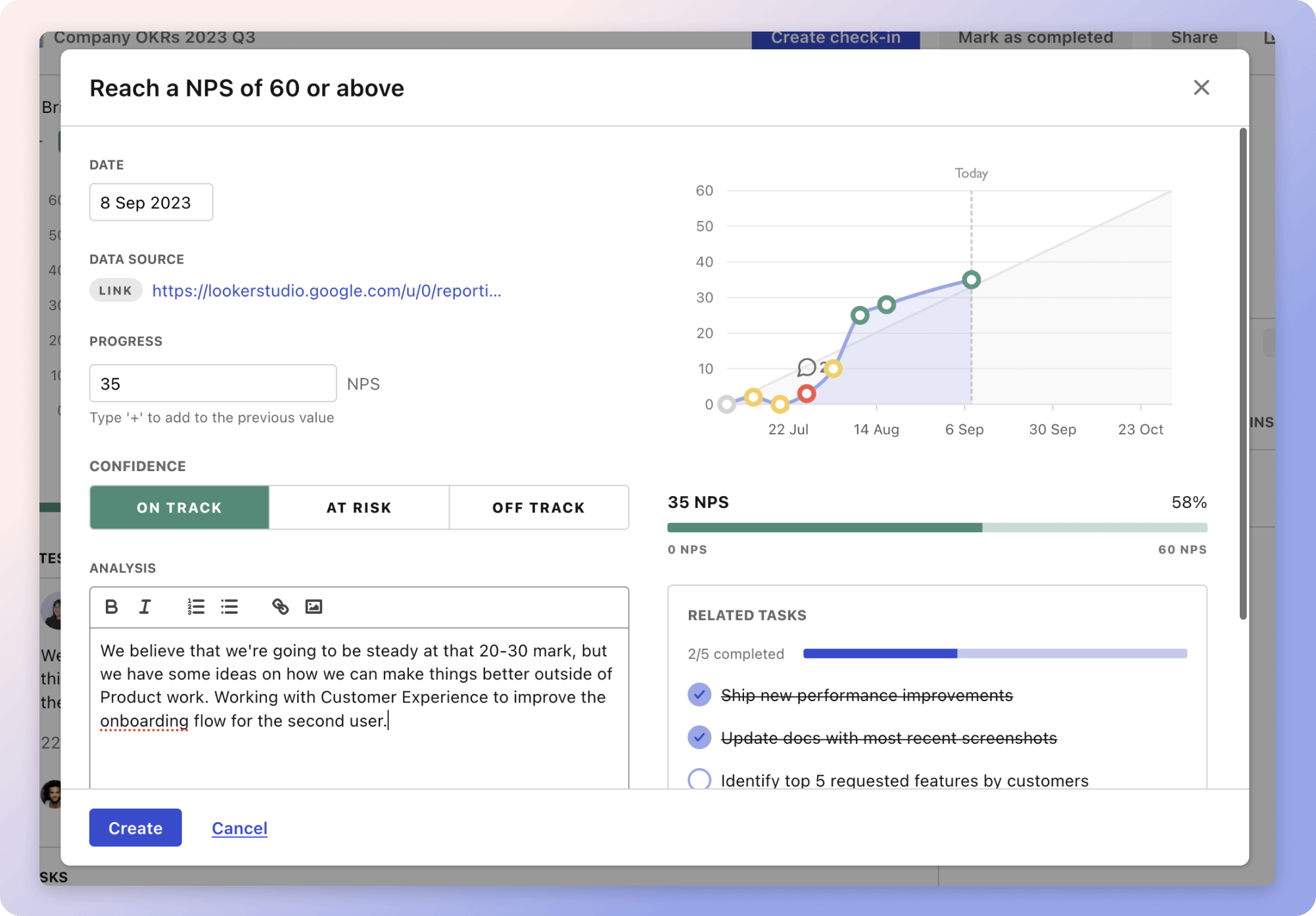 Tability's check-ins will save you hours and increase transparency
Tability's check-ins will save you hours and increase transparencyThe best metrics for Routine Staff Training
The best metrics for Data Uptime Measurement
The best metrics for Increasing Revenue and Users
The best metrics for Attract 4 Retainer Clients
The best metrics for Performance Management
The best metrics for Empowering Innovation and Service Delivery