What are Infection Control metrics? Finding the right Infection Control metrics can be daunting, especially when you're busy working on your day-to-day tasks. This is why we've curated a list of examples for your inspiration.
Copy these examples into your preferred app, or you can also use Tability to keep yourself accountable.
Find Infection Control metrics with AI While we have some examples available, it's likely that you'll have specific scenarios that aren't covered here. You can use our free AI metrics generator below to generate your own strategies.
Examples of Infection Control metrics and KPIs 1. Sterilisation Cycle Success Rate Percentage of completed sterilisation cycles that meet all protocol standards
What good looks like for this metric: 95% or higher
Ideas to improve this metric Regularly maintain and calibrate sterilisation equipment Conduct routine staff training to ensure proper procedures are followed Implement regular audits of sterilisation processes Adopt real-time monitoring systems for sterilisation equipment Establish a clear protocol for dealing with failed cycles 2. Infection Rates Post-Procedure Rate of infections related to procedures involving reusable instruments
What good looks like for this metric: Below 0.5%
Ideas to improve this metric Ensure strict adherence to sterilisation protocols Improve hand hygiene compliance among staff Regularly update the infection control policy Conduct regular staff training on infection prevention Implement a thorough post-sterilisation instrument inspection process 3. Instrument Cleaning Time Average time taken for cleaning instruments prior to sterilisation
What good looks like for this metric: 15-30 minutes
Ideas to improve this metric Streamline cleaning procedures to reduce time Ensure proper staffing levels in the cleaning area Invest in advanced cleaning equipment Regularly train staff on efficient cleaning practices Schedule regular audits of cleaning processes to identify bottlenecks 4. Equipment Downtime Total time sterilisation equipment is non-functional
What good looks like for this metric: Less than 5%
Ideas to improve this metric Implement a preventative maintenance schedule for equipment Keep a log of equipment issues to identify recurring problems Train staff in basic troubleshooting to minimise downtime Have spare parts on hand for quick repairs Choose high-quality equipment with a reliable service contract 5. Compliance With Sterilisation Protocols Rate of adherence to established protocols by staff during sterilisation procedures
What good looks like for this metric: 100%
Ideas to improve this metric Provide regular training sessions on sterilisation protocols Conduct random audits to ensure compliance Encourage a culture of safety and protocol adherence Implement a feedback system for continuous improvement Use role-play scenarios to prepare staff for protocol deviations
← →
1. CLABSI Incidence Rate The number of central line-associated bloodstream infections per 1,000 central line days
What good looks like for this metric: Typical rates are below 1.0 per 1,000 line days
Ideas to improve this metric Ensure adherence to insertion and maintenance protocols Conduct routine infection control training for staff Implement a checklist for central line insertion Review and enhance hand hygiene adherence Utilise antimicrobial-impregnated catheters 2. Central Line Utilisation Ratio The proportion of patient days for which central lines are used
What good looks like for this metric: Aim for a ratio below 0.5
Ideas to improve this metric Assess necessity of central lines daily Opt for alternative access methods when possible Educate staff on risks of unnecessary central line usage Implement daily rounds to evaluate central line need Standardize criteria for central line removal 3. Hand Hygiene Compliance Rate The percentage of times hand hygiene is properly performed as per the protocol before and after handling central lines
What good looks like for this metric: Target compliance rate of ≥90%
Ideas to improve this metric Install hand hygiene stations near patient beds Use electronic monitoring systems for hand hygiene Conduct regular compliance audits Provide feedback to staff on hand hygiene performance Introduce incentives for high compliance rates 4. Catheter Duration Average duration (in days) central lines are kept in place
What good looks like for this metric: Strive for minimal duration necessary for patient care
Ideas to improve this metric Review catheter need daily with a multidisciplinary team Set standard guidelines for acceptable catheter duration Promote patient involvement in daily catheter necessity evaluation Train staff to identify early signs of infection Utilize IT solutions to track catheter data and prompt removal 5. Staff Training Hours on CLABSI Prevention The total number of training hours completed by staff on preventing CLABSI annually
What good looks like for this metric: Minimum of 10 hours per staff member annually
Ideas to improve this metric Schedule regular training sessions throughout the year Incorporate e-learning modules for flexible access Engage staff with simulation-based learning Utilise external experts for specialized training Evaluate training effectiveness with pre- and post-tests
← →
1. Central Line-Associated Bloodstream Infections (CLABSI) Rate This metric calculates the number of CLABSIs per 1,000 central line days in a healthcare setting
What good looks like for this metric: 0.8 infections per 1,000 central line days
Ideas to improve this metric Enhance hand hygiene protocols Utilise aseptic techniques during insertion Conduct regular staff training on line care Implement daily reviews of line necessity Use antimicrobial or antiseptic impregnated catheters 2. Compliance with Central Line Bundle The percentage of adherence to a proven protocol bundle that reduces infection risk during central line placements
What good looks like for this metric: 95% compliance
Ideas to improve this metric Standardise use of full barrier precautions Ensure appropriate skin antiseptic application Optimise the line insertion site based on risk Introduce audits and feedback systems Train staff regularly on bundle compliance 3. Central Line Duration The average number of days a central line remains in place
What good looks like for this metric: 5-7 days
Ideas to improve this metric Regularly assess the necessity of each line Establish protocols for early removal Increase awareness through patient education Develop an interdisciplinary line management team Use checklists to monitor line use 4. Infection Rate Post-Line Removal Measures the incidence of infection detected within 48 hours post-central line removal
What good looks like for this metric: Below 5%
Ideas to improve this metric Monitor signs of infection post-removal Improve patient follow-up procedures Offer training on signs of potential complications Educate patients on post-removal care Investigate and address removal technique issues 5. Patient Improvement Post-Implementation Tracks the improvement in patient health outcomes following the implementation of infection control measures
What good looks like for this metric: Improvement rate above 90%
Ideas to improve this metric Collect and analyse patient feedback Regularly update infection control protocols Introduce new control measures based on data Facilitate a collaborative care approach Invest in continuous staff development
← →
1. Infection Rate Reduction The measure of reduction in infection cases reported in the facility after renovations
What good looks like for this metric: A typical benchmark is a 20% reduction in infection rates
Ideas to improve this metric Conduct regular infection audits Ensure proper sanitisation of equipment Implement staff training on infection control Enhance air filtration systems Utilise antimicrobial surfaces 2. Patient Safety Incident Count Number of safety-related incidents reported per 1,000 patient days
What good looks like for this metric: Aim for fewer than 10 incidents per 1,000 patient days
Ideas to improve this metric Standardise safety protocols Improve staff communication channels Introduce safety drills and training Enhance surveillance systems Regularly update safety guidelines 3. Workflow Efficiency Percentage Percentage of processes completed within the expected time frame
What good looks like for this metric: Achieving at least 85% on-time process completion
Ideas to improve this metric Optimise staffing schedules Implement workflow management software Regularly review and adjust processes Conduct time management training Utilise feedback to streamline operations 4. Patient Satisfaction Scores Patients' average satisfaction rating post-renovation
What good looks like for this metric: A target of at least 90% satisfaction
Ideas to improve this metric Enhance waiting area conditions Provide clear communication about changes Solicit frequent patient feedback Ensure staff are attentive and responsive Provide patient education on safety improvements 5. Staff Compliance Rate with Protocols Percentage of staff compliance with updated infection control protocols
What good looks like for this metric: Aim for at least 95% compliance
Ideas to improve this metric Incentivise adherence to protocols Conduct regular staff assessments Provide ongoing training sessions Utilise visual reminders and aids Implement a peer review system
← →
1. Infection Rate The percentage of patients who develop infections at the surgical site after caesarean delivery.
What good looks like for this metric: Less than 2% infection rate
Ideas to improve this metric Implement strict sterilisation protocols Apply appropriate wound dressing techniques Ensure proper hand hygiene among staff Use prophylactic antibiotics when appropriate Conduct regular infection surveillance 2. Average Length of Stay The average number of days patients remain hospitalised post-caesarean, which can indicate complications such as infections.
What good looks like for this metric: 3-4 days
Ideas to improve this metric Streamline discharge planning processes Enhance post-operative care and monitoring Provide patient education on self-care post-discharge Utilise early patient mobilisation techniques Increase follow-up care frequency 3. Readmission Rate The percentage of patients readmitted due to surgical site infections following initial discharge after caesarean.
What good looks like for this metric: Less than 5% readmission rate
Ideas to improve this metric Conduct thorough post-discharge evaluations Educate patients on infection warning signs Implement a robust follow-up appointment system Enhance patient communication channels Ensure high-quality home care instructions 4. Wound Healing Time The average time it takes for surgical wounds from caesarean sections to heal completely.
What good looks like for this metric: 4-6 weeks
Ideas to improve this metric Enhance patient nutrition and hydration Provide effective pain management options Regularly assess the wound for signs of infection Implement advanced wound care therapies Promote patient compliance with care instructions 5. Patient Satisfaction Score The level of patient satisfaction regarding their post-operative care and outcomes.
What good looks like for this metric: Above 85%
Ideas to improve this metric Improve patient communication and engagement Provide thorough pre-operative education Ensure empathetic and supportive nursing care Empower patients with self-care knowledge Incorporate patient feedback into care plans
← →
1. Hand Hygiene Compliance Rate The percentage of times clinical staff wash their hands following recommended guidelines
What good looks like for this metric: 80% compliance rate in healthcare settings
Ideas to improve this metric Implement regular staff training on hand hygiene Install more hand sanitiser dispensers Conduct random audits and provide immediate feedback Use visual cues or posters to remind staff Introduce a reward system for compliance 2. Contamination Incidence Rate The number of contamination events reported per 1,000 patient days
What good looks like for this metric: Less than 2 events per 1,000 patient days
Ideas to improve this metric Conduct thorough root cause analysis for each event Increase frequency of sanitation checks Enhance the usage of personal protective equipment Involve staff in contamination prevention strategies Regularly review and update infection control policies 3. Waste Segregation Accuracy Percentage of waste correctly segregated into appropriate categories
What good looks like for this metric: 95% correct segregation
Ideas to improve this metric Provide clear, colour-coded bins and labelling Train staff on waste segregation procedures Conduct waste audits to assess segregation accuracy Incorporate waste management into annual assessments Implement accountability measures for non-compliance 4. Staff Training Completion Rate Percentage of clinical staff who have completed required hygiene and waste management training
What good looks like for this metric: 100% completion annually
Ideas to improve this metric Schedule mandatory training sessions at convenient times Use online platforms for training flexibility Track and remind staff of training deadlines Encourage peer-to-peer knowledge sharing Provide certificates upon completion to acknowledge achievement 5. Patient Satisfaction Scores Related to Cleanliness Patient feedback scores on cleanliness and hygiene aspects of care
What good looks like for this metric: 4.5 out of 5 in patient satisfaction surveys
Ideas to improve this metric Solicit regular patient feedback and act on suggestions Improve visibility of cleaning efforts Ensure high-touch surfaces are sanitised frequently Engage patients in dialogue about hand hygiene Reward staff for high cleanliness scores
← →
Tracking your Infection Control metrics Having a plan is one thing, sticking to it is another.
Setting good strategies is only the first challenge. The hard part is to avoid distractions and make sure that you commit to the plan. A simple weekly ritual will greatly increase the chances of success.
A tool like Tability can also help you by combining AI and goal-setting to keep you on track.
More metrics recently published We have more examples to help you below.
Planning resources OKRs are a great way to translate strategies into measurable goals. Here are a list of resources to help you adopt the OKR framework:
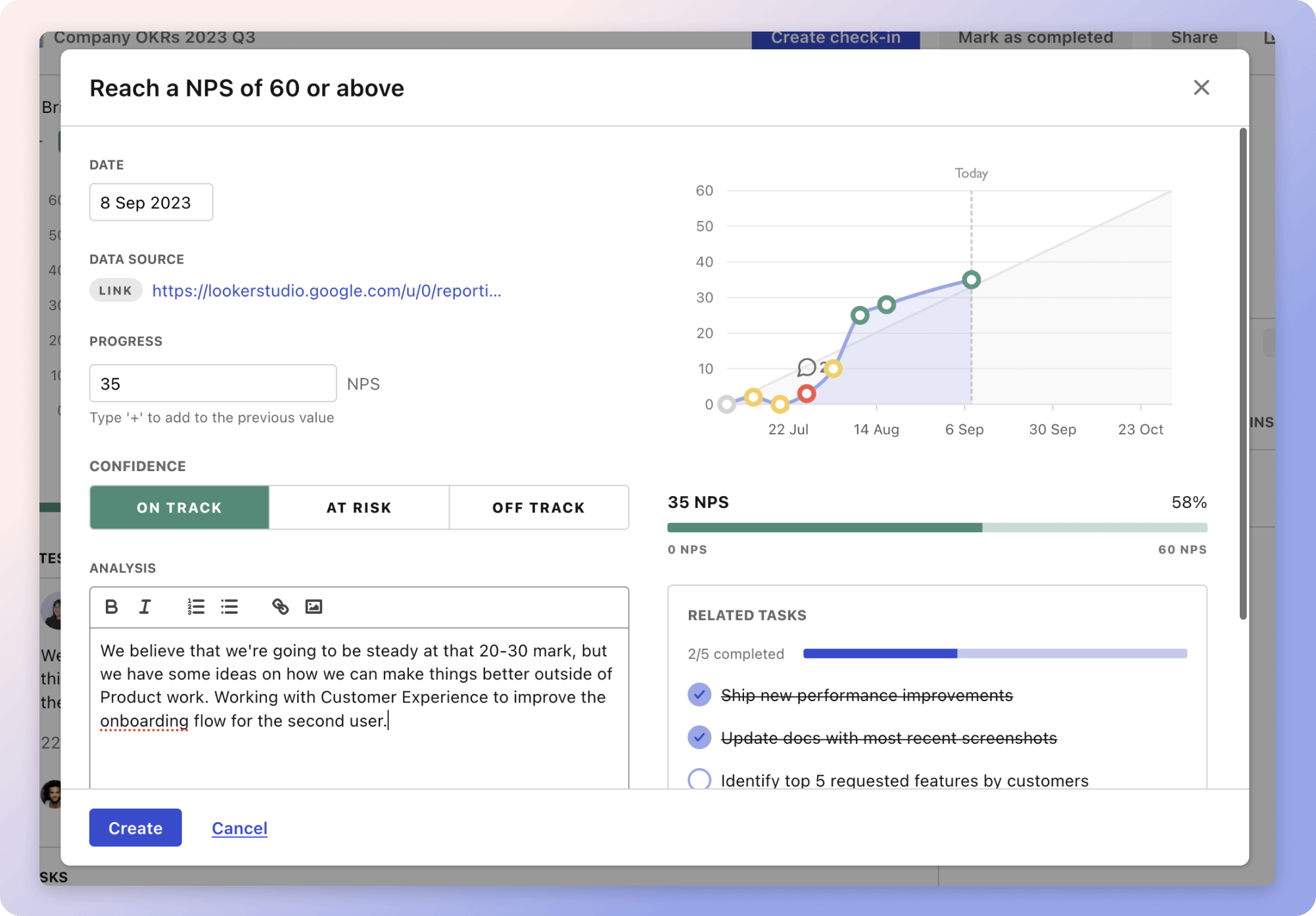 Tability's check-ins will save you hours and increase transparency
Tability's check-ins will save you hours and increase transparencyThe best metrics for Routine Staff Training
The best metrics for Data Uptime Measurement
The best metrics for Increasing Revenue and Users
The best metrics for Attract 4 Retainer Clients
The best metrics for Performance Management
The best metrics for Empowering Innovation and Service Delivery